Driving Awareness for Relapsing Polychondritis
Race for RP is a partnership with race car drivers, teams, owners, sponsors, and enthusiasts to drive awareness and accelerate research for relapsing polychondritis (RP) and other autoimmune diseases. Race for RP is the motorsports initiative that supports the work of the Relapsing Polychondritis Foundation. The RP Foundation is a non-profit organization that invests in RP related research and awareness programs with the goal of improving the care of those affected by relapsing polychondritis and related autoimmune diseases.
What is Relapsing Polychondritis?
The Impact of Relapsing Polychondritis
Not much is known about this rare and degenerative autoimmune disease that afflicts millions of people. That’s why we invest in research to better understand and treat it.
5,000
Number of people in the U.S. with Relapsing Polychondritis
50/50
Relapsing Polychondritis impacts men and women equally
40-60
Age most people begin experiencing symptoms
1 of 150





Fueling Groundbreaking RP-Focused Research
The Race for RP and the Relapsing Polychondritis Foundation are accelerating research and studies to help diagnose, prevent and cure relapsing polychondritis and related autoimmune diseases. Together with our talented collaborative research partners, we are driving RP and autoimmune diseases to the forefront of ground-breaking discoveries. We are also improving patient access to specialized, multi-disciplinary teams of clinicians and are fostering a greater understanding of RP among clinicians, scientists and the broader community. We recognize the vital need for funding to support the next wave of progress and sustain the important research that’s forging the path to a cure.
Research projects and studies, and growing
Collaborative research partners (so far)
HELP US DRIVE DISCOVERIES. PARTICIPATE IN OUR EXCITING, INNOVATIVE FUNDRAISING EVENTS.
VIP Race Weekend, May 24-27, 2024
Get immersed in the action of and exclusive celebrations for the 108th running of the Indianapolis 500!
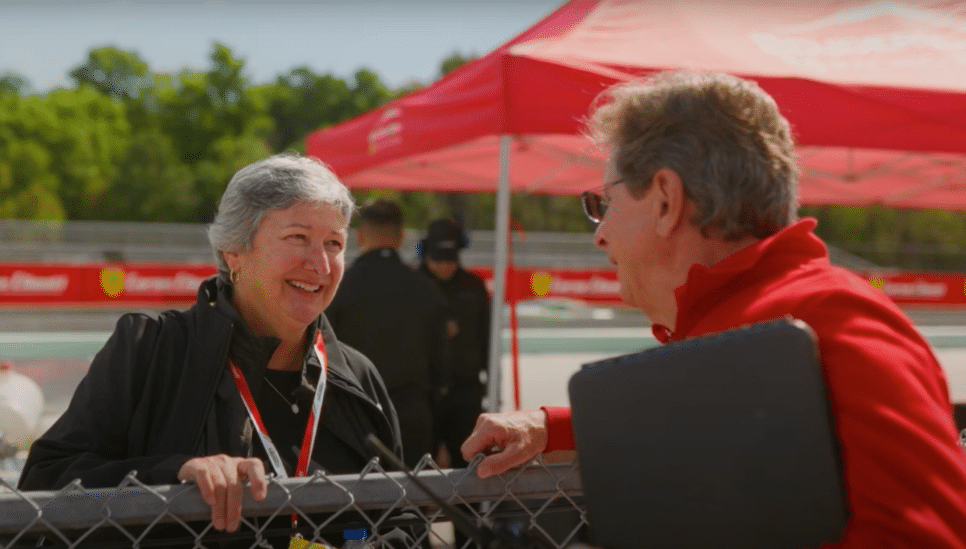
The founding of race for RP
Race for RP’s inception comes from Nancy Linn’s story. After years of painful and debilitating symptoms with no clear cause, Nancy was diagnosed with relapsing polychondritis. She found strength and the courage to persevere by choosing to live with purpose. Race for RP raises awareness about RP in clinical, scientific, and broader community arenas, and advances research efforts for this and other autoimmune diseases to catalyze discoveries that improve diagnosis, patient outcomes, and ultimately, lead to a cure. With countless other patients afflicted with autoimmune disease and facing similar struggles, Nancy’s purpose is our collective purpose.
Watch Trailer: "The Race Of Our Lives"
Discover how your support fuels the RP Foundation’s mission and energizes a community dedicated to changing the outcomes for patients with RP and related autoimmune diseases.
Playing Now: "The Race Of Our Lives"

Race for RP Today
We have never lost sight of our purpose and have become a catalyst for awareness and research on treatments and cures for relapsing polychondritis and related autoimmune diseases.
News About Relapsing Polychondritis